By Motion Physical Therapist: Dr. Alyssa George, PT, DPT, OCS
If you have ever experienced a fall and landed on your tailbone, you know how painful this can be. Winter here in Minnesota lends itself to icy sidewalks that can quickly find us on the ground, landing directly on this sensitive structure. Your coccyx (tailbone) is a small triangle-shaped bone located at the base of your spine and functions as a segment for muscle, tendon, and ligament attachments. These muscles and ligaments are important for helping to support the pelvic floor for normal bowel movements and bladder and sexual function. The coccyx is also an important weight-bearing structure along with your “sit bones” that shares some of the weight when we sit. We spend on average, 29.7% of our lives sitting!1 Having a painful coccyx can really impact a person’s quality of life. It is most commonly injured from external trauma such as a fall or internal trauma from delivering a baby. Women are 5 times more likely to develop coccyx pain than men.2 Conservative treatment is successful in 90% of cases, and many resolve without medical treatment.3 This treatment can include using a cushion, changing your posture, using heat/cold or over the counter anti-inflammatory medications, or going to physical therapy. In general, management of coccyx pain involves the following:
1. Posture
Avoid slump sitting which puts pressure on your tailbone. Lean more forward while sitting up straighter and this should take pressure off of your tailbone. Place a towel roll behind your low back as a reminder to avoid slumping. Sitting on a firmer surface may be better than a soft, cushy couch which often encourages slump sitting. Many people will try to sit off to one side to take pressure off of the tailbone. This is not a good strategy and can cause more pelvic issues so it is best to just sit more forward with even weight on both sides of the pelvis. A wedge-shaped cushion with the back section cut out is usually what I recommend.
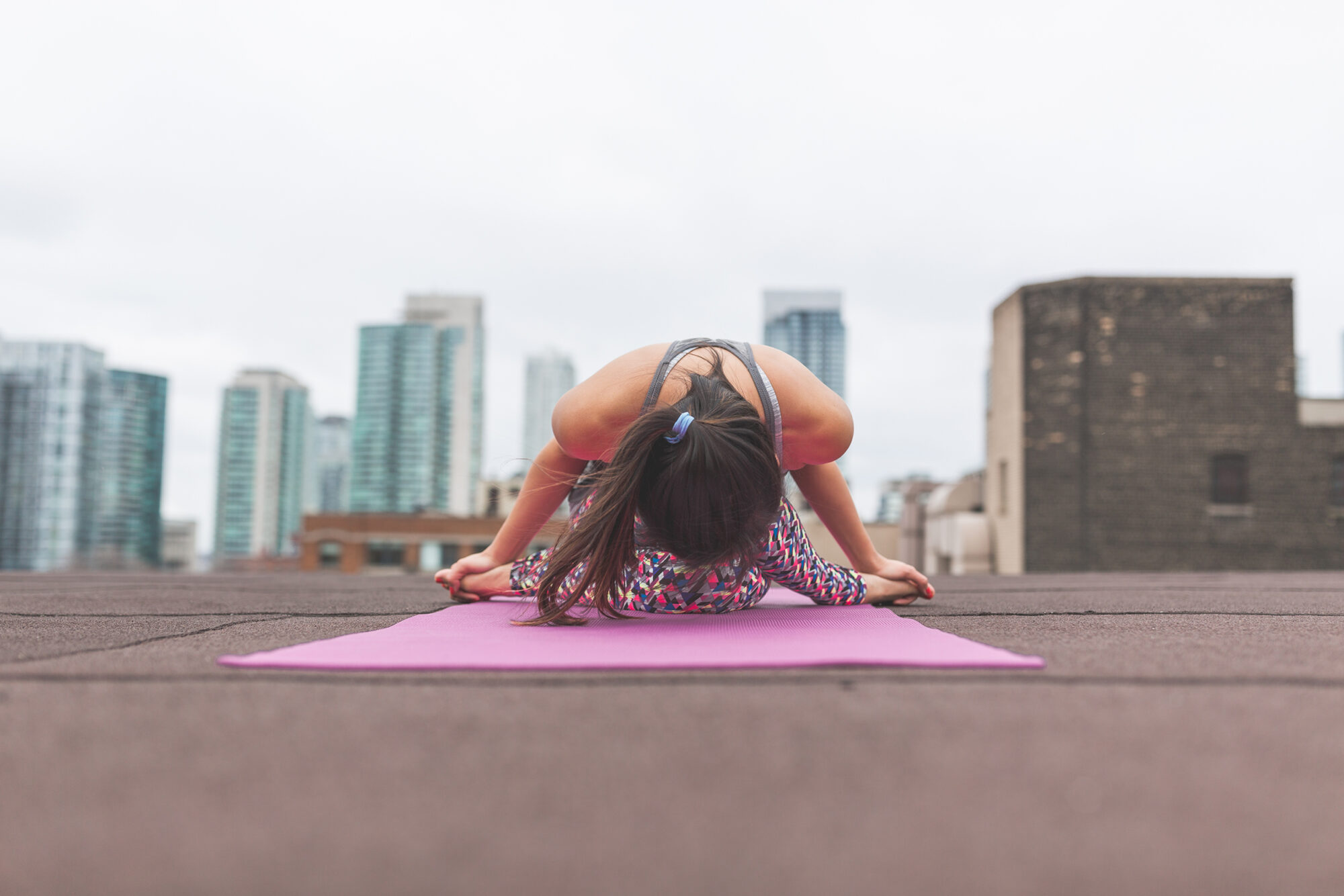
2. Stretches
It may be helpful to stretch the area around your tailbone by doing a “child’s pose” stretch with your hips wide or lying on your back and pulling both knees to your chest. Another option would be to perform a deep squat. In any of these positions, think about relaxing the area around the tailbone and between your sit bones (aka “the pelvic floor muscles”) and focus on deep breathing. Frequently check in with these muscles throughout the day to make sure you are not holding excess tension here which is a common compensation when our bodies feel like they need to protect the area after injury.
3. Pelvic Floor Physical Therapy Treatment
Can assist with reducing muscle spasms and assess for the mobility and position of the sacrococcygeal joint. The goal is always to reduce pain and sensitivity of the tissues and restore mobility of the coccyx, sacrum, and lumbar spine if indicated. This may involve soft tissue mobilization, joint mobilization, or dry needling. Additional treatments may involve focused strengthening exercises or using a taping technique to help support the manual techniques performed. In general, if coccyx pain has not resolved after a few weeks of the initial injury, it may be necessary to make an appointment with a pelvic floor physical therapist.
Dr. Alyssa George, PT, DPT, OCS

Alyssa wants to get you back to doing what you love, whether that be sports/recreational activities, your career, or caring for your family. Specializing in treating pelvic and orthopedic conditions, Alyssa develops individualized treatment plans because she understands that no two bodies are alike. She has been involved in research projects to help advance the field of physical therapy. Most recently she has written a case series detailing the benefits of dry needling for chronic pelvic pain and presented on the function of breathing muscles in pelvic pain at the American Physical Therapy Association’s Combined Sections Meeting. She has over nine years of experience as a physical therapist and has started and led pelvic health programs at clinics in Texas, Ohio, and now Minnesota, her home state.
Alyssa earned a Bachelor of Arts degree in biology from Gustavus Adolphus College, a Master of Physical Therapy degree from the University of Wisconsin-Madison, and continued her education at the University of Montana, earning her Doctorate in Physical Therapy. She is a board-certified clinical specialist in orthopedics and earned her certification in pelvic physical therapy from the American Physical Therapy Association Section on Women’s Health. She has been a lecturer and faculty mentor of both orthopedic residency and manual therapy fellowship programs at The Ohio State University and is a credentialed clinical instructor for physical therapy students. Alyssa has been certified in dry needling and utilizes other various manual therapy techniques in her management of abdominopelvic disorders (including incontinence, constipation, lumbopelvic pain, and pregnancy-related musculoskeletal disorders) and orthopedic conditions of the neck, back, shoulder, hip, knee, and foot/ankle.
Schedule an Appointment with Dr. Alyssa Today for a More In-Depth Assessment
References
- http://news.reebok.com/global/latest-news/reebok-survey–humans-spend-less-than-one-percent-of-life-on-physical-fitness/s/aaf2c121-6889-40fd-a0dc-ba64b64cc85a
- Maigne JY, Doursounian L, Chatellier G. Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Spine (Phila Pa 1976) 2000 Dec 1;25(23):3072–3079. [PubMed]
- Thiele GH. Coccygodynia: Cause and treatment. Dis Colon Rectum. 1963 Nov-Dec;6:422–436. [PubMed]